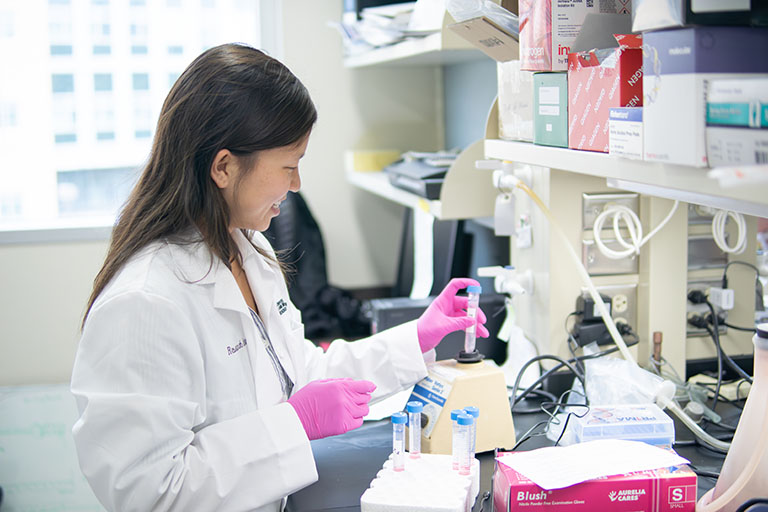
Research cures cancer
Did you know that the cure for testicular cancer was discovered at Indiana University? In fact, we celebrated the 50th anniversary of that medical milestone at the end of 2024.
That’s just one of the life-saving breakthroughs at IU Melvin and Bren Simon Comprehensive Cancer Center—and that’s just one of the reasons why we’re the only National Cancer Institute-designated comprehensive cancer center in Indiana and one of only 57 in the nation. Plus, because we’re one of only 33 members of the National Comprehensive Cancer Network, our physicians play a role in determining the recognized standard of care for those with cancer.
We’re doing some really exciting things around here. Get ready to be astonished.