For many years, the fight against multiple myeloma unfolded like a siege—slow gains measured against painful losses.
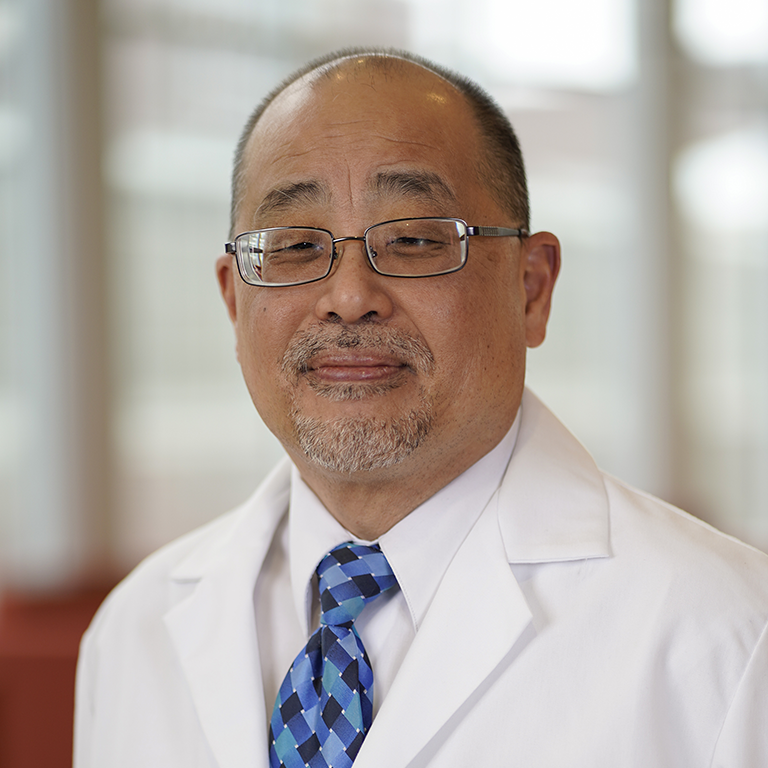
Now, researchers like Rafat Abonour, MD, speak optimistically about what the future holds. “A lot of us are bold enough to say we can cure multiple myeloma with the treatment we provide,” said Abonour, who oversees the myeloma program at Indiana University Melvin and Bren Simon Comprehensive Cancer.
Since 2013, eight therapies have gained federal approval, including second-generation proteasome inhibitors and newer immune-based options like bispecific antigens. Those advances have provided oncologists with a deeper bench of options for patients whose disease requires second or third options. For some, care for managing myeloma resembles managing a chronic condition.
Yet researchers still tackle thorny problems.
Why do some patients with precursor conditions like smoldering multiple myeloma or monoclonal gammopathy of undetermined significance (MGUS) eventually progress to full-blown cancer? Why does myeloma surge back–even if immunotherapy wipes it out? What genetic factors power hyper-aggressive disease?
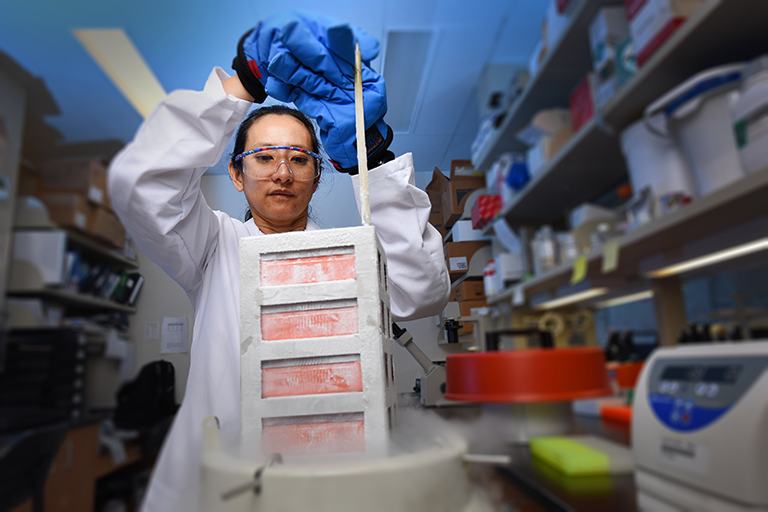
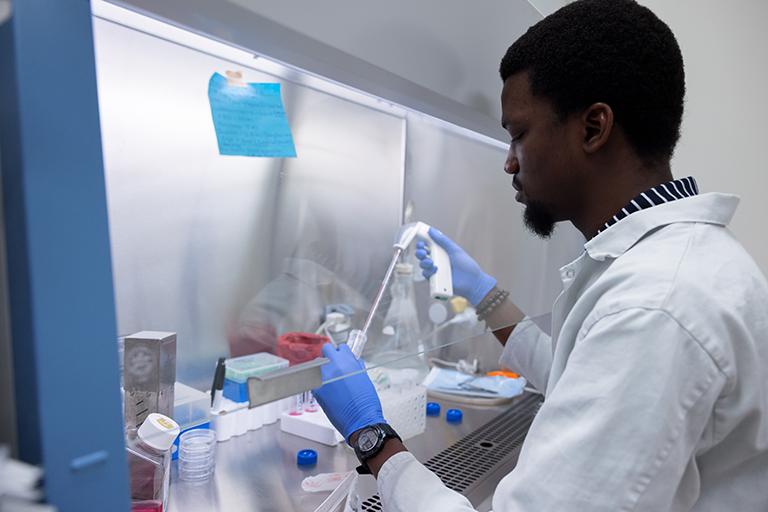
At the IU Simon Comprehensive Cancer Center, we are striving to find those answers. Our physicians and researchers work at the cutting edge, using the latest advances in genomic sequencing, machine learning and drug discovery. They also lead clinical trials for the newest options in immunotherapy.
Our progress against multiple myeloma is also made possible by generous donors like you.
“Donors have helped us build a strong program,” Abonour said. “It’s given us opportunities to be bold. We can ask big questions. Sometimes, doing that means you won’t get funded through traditional sources.”
Philanthropy will allow the IU Simon Comprehensive Cancer Center to continue to recruit talented scientists. It will underwrite collaborations with the Brown Center for Immunotherapy, turning newly discovered targets into immunotherapies manufactured at IU. And it can fund trials offering new therapies through IU Health’s statewide network.
Together, we can reach the ambitious goal of curing myeloma. Here is a look at our progress and what supporters make possible.