At the Indiana University Melvin and Bren Simon Comprehensive Cancer Center, a team of more than 30 scientists at our Tom and Julie Wood Center for Lung Cancer Research is taking on lung cancer from every angle. Our researchers are working to improve prevention efforts, detect lung cancer earlier and develop personalized therapy to improve the standard of care for lung cancer treatments.
While we are making meaningful progress, one fact remains: more people in the United States die from lung cancer than any other type of cancer.
Fortunately, we have you. Our donors are critical partners, making investments that lead to breakthroughs. Together, we’re making progress that will save lives in Indiana and around the world. Here is a glimpse of what you make possible.
Lung Cancer Research Update
Culture of collaboration and team science

Established in March 2024, the Tom and Julie Wood Center for Lung Cancer Research continued to gain momentum in 2025 when it named John Turchi, PhD, its inaugural executive director. Turchi’s leadership is shaping a collaborative approach to lung cancer research, from our labs to clinical application.
The Wood Center is focusing on three key pillars in its research efforts:
- Developing new therapies to treat lung cancer;
- Examining how exposures such as cigarette smoke, occupational factors and air pollution impact lung cancer development; and
- Looking at predictive biomarkers of lung cancer development, the responses to cancer therapies, while advancing lung cancer screening.
Clinical trials and advances
An IU study in patients with early-stage lung cancer could help determine who may benefit from additional treatment after surgery. The study, led by Nasser Hanna, MD, followed patients who underwent surgery, then chemotherapy and immunotherapy. Researchers conducted periodic blood draws to evaluate whether cancer DNA, which is an indicator of residual disease, could be detected following treatments.
Rohan Maniar, MD, shared initial findings this year at an international conference. The IU research team demonstrated that the absence of cancer DNA correlated with a lack of cancer recurrence. In cases where cancer DNA persisted, clinicians were able to clear it with additional therapy—a precision-based approach that may have been lifesaving for those patients.
About 35,000 patients are diagnosed with stage I lung cancer annually in the United States. The current standard of care for these patients with early-stage disease is surgery and then observation – with a five-year overall survival of 73-86%.
IU researchers want to know if treatment after surgery with a specific immunotherapy called pembrolizumab will improve survival rates for these patients. To answer this question, Greg Durm, MD, is leading a randomized clinical study that opened first at IU and is now offered at centers across the country.
Durm is also working to open a study using a wearable device—called tumor treating fields device—that is designed to disrupt cancer cell division. The therapy has been used in glioblastoma and pancreatic cancers. Now researchers want to see if the device can improve outcomes for lung cancer patients.
Shadia Jalal, MD, the Lawrence H. Einhorn Professor of Oncology, is examining the impact of fasting in combination with immunotherapy for patients with advanced non-small cell lung cancer. The goal is to explore whether fasting can enhance the effectiveness of immune-based treatments. Jalal also is leading a biomarker-directed trial in small cell lung cancer and relapsed small cell lung cancer. This trial aims to personalize treatments based on molecular markers.
Early detection and screening

Thanks to a generous gift from the Tom and Julie Wood Family Foundation, Indiana’s first mobile lung cancer screening program launched in 2025, taking life-saving screenings to eligible high-risk Hoosiers statewide. The mobile program, part of the End Lung Cancer Now initiative, has already visited more than 35 Indiana counties in its first eight months.
Early detection through low-dose CT scans could decrease lung cancer’s mortality rate by 20%. That’s why early detection and screening is vital. The mobile program is just one of the ways IU researchers are working to improve early detection and screening. The lung screening research working group brings together a wide range of research expertise including radiology, pulmonary medicine, cardio-oncology, artificial intelligence and basic science.
Nasser Hanna, MD, the Tom and Julie Wood Family Foundation Professor of Lung Cancer Clinical Research, is leading studies to improve outcomes for patients receiving lung screenings. One study, co-led by Josh Rager, MD, is looking at outcomes for patients who receive screenings at a mobile lung program compared to a traditional program in a hospital or clinic.
Another project, co-led by Natalia Rodriguez, PhD, aims to assess the feasibility of performing lung screening in a population of people experiencing homelessness. Additionally, Hanna and Julian Marin-Acevedo, MD, are leading a study that aims to expand the eligibility criteria for high-risk individuals who are not currently eligible for lung cancer screening.
Understanding how cancer develops
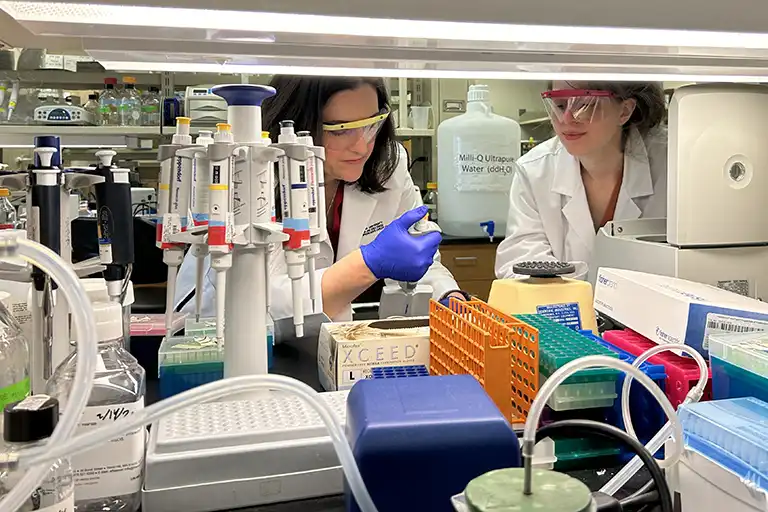
Catherine Sears, MD, is leading research into the earliest stages of lung cancer development, with a focus on how DNA repair and environmental exposures ultimately lead to lung cancer. Her lab is expanding its studies on how deficiencies in DNA repair contribute to the transition from precancerous to cancerous lung lesions.
Sears is exploring pollution-related lung cancer, which includes risks such as from occupational exposures, wildfires and military burn pits. Her lab is investigating how DNA repair mechanisms may be impacted by pollution exposure, and how this contributes to development of lung cancer and other associated lung diseases.
Lung cancer screening is available for those who meet current screening criteria, and it saves lives. Nearly half of lung cancer patients fall outside of current lung screening guidelines, because screening is limited to exposures related to smoking. Dr. Sears’ research may ultimately identify those who are at an increased risk for lung cancer to improve screening and prevention, particularly for those at higher risk due to non-classic exposures who do not currently meet the lung screening guidelines.
Sears and Nawar Al Nasrallah, MD, are investigating DNA repair capacity as a biomarker for lung cancer and other lung diseases. The study collects blood and tissue samples from people to assess whether reduced repair capacity occurs before cancer development.
Additionally, Al Nasrallah is advancing lung cancer research with his efforts to understand aging, DNA repair and age-related diseases. DNA repair is a critical process to maintain stability in cells, but that process becomes less efficient as the body ages. His research is exploring how this diminished DNA repair capacity contributes to aging-related lung diseases, including cancers. The study is also exploring how lifestyle factors—such as diet and exercise—that may influence DNA repair and disease risks.
Clinical innovations
Misty Shields, MD, PhD, is working on biomarker identification in small cell lung cancer. Her lab has identified a novel protein that may predict durable response to an FDA approved medication called lurbinectedin, and her lab is studying the role of this biomarker in small cell lung cancer.
Turchi, who serves as the Tom and Julie Wood Family Foundation Professor of Lung Cancer Research, has proven in models that his lab’s promising drug target, called Ku, has anti-cancer efficacy in combination with radiation. The Turchi lab has been developing this compound for more than a decade, and this proof-of-concept model moves it closer to a clinical trial for non-small cell lung cancer.
The Turchi lab is advancing its project focused on a protein called replication protein A (RPA), working toward an FDA drug application for an RPA-targeted drug therapy, while optimizing a version of the drug that can be taken orally.
Since 2023, Shields has been leading a study to collect liquid biopsies—meaning samples such as blood—during patients’ journeys with small cell lung cancer. Patients consent to the study shortly after diagnosis, and then they are followed through each line of therapy with collections occurring at their scan visits.
The study seeks to identify treatment resistance that may occur in limited-stage or extensive-stage small cell lung cancer, so researchers can target that resistance mechanism with new therapies. These samples are studied for DNA, RNA and protein changes, neuroendocrine subtypes, and clinical outcomes such as toxicities and response on imaging.
In the quest to revolutionize lung cancer treatment, some of our patients provide the most precious gift to research—themselves. These patients have consented to a biopsy to donate tissue within 12 hours of their death.
Led by Jalal, this tissue biorepository is invaluable for researchers. Using collected samples, researchers are analyzing mechanisms of treatment resistance and the varied subpopulations of cancer cells within small-cell lung cancer.
Looking to 2026, the IU lung cancer team is working to open a broad range of trials that will include options for nearly every lung cancer diagnosis, including small cell and non-small cell types. Every bold idea in the lab and new trial in the clinic is momentum toward taking down lung cancer for Hoosiers and beyond.
Support the Future of Lung Cancer Research
Your support is crucial in helping IU Simon Comprehensive Cancer Center find solutions for America’s leading cause of cancer deaths.
For other ways to support lung cancer research, contact Amber Kleopfer Senseny at 317-278-4510 or akleopfe@iu.edu.




